Salmonellosis caused by Salmonella is one of the most unpleasant food borne diseases we can suffer. It was described back in 1984 as a ‘new and significant threat to public health’ by the World Health Organisation. There is nothing to suggest this claim has been reduced over the years. It is associated with a wide variety of foods and probably sits up there with botulism as one of those diseases that causes most fear (Crim et al., 2014; EFSA-ECDC, 2015).
Salmonellosis causes mild to moderate gastroenteritis, resulting in diarrhea, abdominal cramps, vomiting and sickness and fever (NIAD, 2007). It is often fatal in young children, the elderly and those with weakened immune systems. Sickness occurs within 12 to 72 hours after eating the food contaminated with the bacteria. The bacteria multiply in the gut and produces diarrhoea when the bacteria penetrate the intestinal cell wall. The endotoxin released on cell death probably produces the fever associated with the disease.
The only other pathogen that appears to cause so much concern is Clostridium botulinum and Listeria.
Historical References To Salmonellosis
Historical studies suggest the Aztecs living in what is today southern Mexico suffered from the disease between 1545 and 1550. The disease was known as cocoliztli. Examination of the DNA of ten different individuals buried at the only known burial site of Teposcolula-Yucubdaa contained Salmonella enterica—subset Paratyphi C.
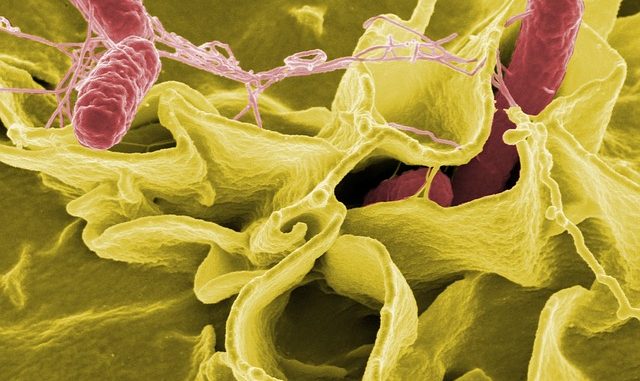
The cause, the Salmonellae, are Gram-negative, facultative anaerobic rods and are part of the Enterobacteriaceae family. A new classification system lists the offending species as S. enterica. the sub-species is also called enterica.
Over 2,500 serotypes (also called servars) are known with commonest type being S. Enteridis and S. Typhimurium. Salmonella enterica serotypes probably account for most of the human infections leading to millions of cases of enteric disease (Hur et al., 2012). The current estimate from the CDC web-site is that 1.2 million people in the USA are affected annually.
Any suggestion that a product is contaminated with the bacteria prompts immediate recall of all affected and very often related products.
Routes Of Salmonella Poisoning
The primary sources of Salmonella are the guts or intestinal tract of birds and animals. Ninety per cent of reptiles also carry the bacteria. The majority of the infections come from ingestion of contaminated foods derived from the following:-
- animals,
- birds
- eggs and egg products
- pork, pig meat and associated products such as sausages, salami, pate
- other meats
- baby food
- powdered milk
One of the most worrying elements and cause for increasing concern in contamination and cross-contamination of ready to eat (RTE) products. It also contaminates various fruits such as melons, watermelons and other curcurbits.
Growth Range
- 7 to 47 Centigrade
- generation time is 10 hours at 10 Centigrade
- some forms of salmonella can grow in as acid a pH as 3.8
Regarding food in general, RTE products must be absolutely free of all pathogens of public health concern. In food processing, there is a a zero tolerance policy especially for salmonella which cuts across borders (European Commission, 2005).
Steps Taken To Reduce Contamination
Any batches of food product which have been tested and shown to have the presence of Salmonella are required to be removed from sale. There must be a clear notice informing customers not to eat the products. All products are to be held in quarantine to allow food inspectors to examine the batch and assess the route and distribution of the food product.
Regulations On Salmonella
(1) Regulations In Europe
The European Commission (EC, 2005) has very strict regulations on the presence of Salmonella. In must be absent in a 25g sample for a range of products placed in the market over the course of its shelf-life. These include all minced meats and meat preparations to be eaten raw, for cooked poultry and other meat-based foods, for mechanically separated meat (MSM), food gelatine and collagen, dairy foods that have not been pasteurised, ice-creams, egg products and RTE foods containing raw egg, milk and whey powder, cooked crustaceans and other shellfish, live bivalve molluscs, sea-urchins, sprouted seeds, precut fruit and vegetables, unpasteurised fruit and vegetable juices, dried infant formula and dried dietary foods for medical purposes, and finally dried follow-on formula.
The only time Salmonella is not tested before is when the manufacturing process or the product excludes/eliminates the risk of salmonella. This applies specifically to meat products to be eaten raw, ice-cream,, egg products and RTE products containing egg. The analytical reference method is EN/ISO 6579.
Cases
Year 1984. In the United Kingdom, aspic glaze is contaminated with S. Enteritidis PT4 which leads to 766 cases and two deaths.
In the summer of 2008, 1,442 people across America became ill from eating fresh hot chilli peppers such as jalapenos and tomatoes. The produce was contaminated with the serovar Salmonella Saint-Paul. The peppers originated from Mexico.
Winter 2017-2018 and ongoing
January 2018 Baby milk sold by the French dairy Lactalis has been found to be contaminated with the bacteria. The situation at the factory was uncovered when 35 small children fell ill with Salmonellosis.
The French finance minister is threatening to levy sanctions on supermarkets for selling contaminated milk when they knew there was a risk. Lactalis which is one of the world’s biggest producers of dairy products recalled all products in December 2017 made at the Craon factory in north-west France when they discovered Salmonella. There is currently a ban on products made at the factory.
Shredded coconut has been linked to a widespread US outbreak which has affected 25 people in 13 states. Six people are hospitalised and there are so far no deaths.
Shredded coconut is often found in desserts and macaroons or oatmeal. One source was an Asian-style dessert drink consumed at a restaurant. States affected include California, New York, Oklahoma, Pennsylvania, Florida. The strains identified in the coconut include Salmonella: Javiana, Rissen, and Thompson.
Salmonella Montevideo is found in clover sprouts served in sandwiches which were served at restaurants in Illinois and Wisconsin. Eight people have been affected.
May/June 2018
The U.S. Food and Drug Administration (FDA), Centers for Disease Control and Prevention (CDC), along with state and local officials are investigating a multi-state outbreak of Salmonella Adelaide infections that has sickened 60 people in five Midwestern states. The latest evidence from epidemiology and preliminary traceback evidence has shown that pre-cut melons are the source of this outbreak. The melon has been found in fruit salad mixes. The CDC has recommended that there is potential contamination of fresh cut watermelon, honeydew melon, cantaloupe, and fresh-cut fruit medley products containing any of these melons. Among the 60 people who have become ill, 47 people had information available, and of those 31 cases (66%) have been hospitalized. The illnesses occurred within the period of April 30, 2018 to May 28, 2018. No deaths have been reported. The states affected are Georgia, Illinois, Indiana, Kentucky, Michigan, Missouri, North Carolina, Ohio, and Iowa.
Given the continuing the number of cases of Salmonellosis, it is the food industry which must ensure through diligent food handling practices that the rise is kept to a minimum. Ideally, it should be zero but there is still room for error.
In the last few years there has been a disturbing trend in foodborne outbreaks with wheat flour. There was an outbreak in France in 2022 and then in 2023 pizzas had to be recalled in the USA.
Updated March 2024.
References
Crim, S. M., Iwamoto, M., Huang, J. Y., Griffin, P., Gilliss, D., Cronquist, A. B., et al. (2014). Incidence and trends of infection with pathogens transmitted commonly through food — Foodborne diseases active surveillance network, 10 U.S. sites, 2006–2013. Morbidity and Mortality Weekly Report, 63(15), pp. 328–332
EFSA-ECDC (2015). The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2014. EFSA Journal, 13(12), 4329. http://dx.doi.org/10.2903/j.efsa.2015.4329 [4191 pp.].
European Commission. (2005). EC European Commission Regulation No. 2073/2005 of 15 November 2005 on microbiological criteria for foodstuffs. Off. J. Eur. Union, L338, 1e26. Available from: http://faolex.fao.org/docs/pdf/eur61603.pdf.
[NIAID] Natl. Inst. of Allergy and Infectious Diseases. (2007) Salmonellosis.

Leave a Reply